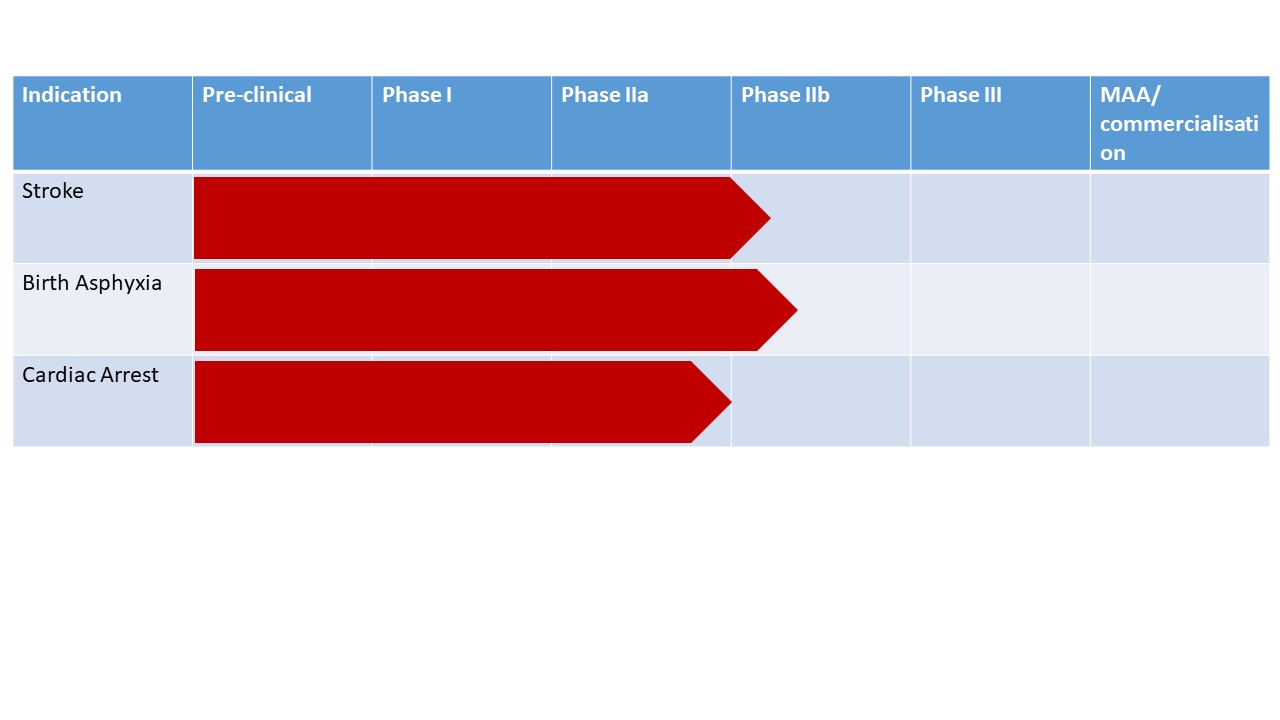
Neurophyxia's main objective is to develop 2-iminobiotin (or 2-IB) a novel injectable pharmaceutical product to reduce the deleterious effects of oxygen shortage (hypoxia-ischemia) in the brain occurring in three life-threatening conditions:
- Stroke
- Cardiac arrest
- Birth asphyxia
The problem: cerebral hypoxia-ischemia and reperfusion injury
Hypoxia-ischemia is a biphasic process in which hypoxia-ischemia and the subsequent reperfusion lead to neuronal cell death over hours to days after the initial insult. Currently, there are no neuroprotective agents available to halt this deleterious process and improve brain function.
The solution: 2-iminobiotin
Our neuroprotective agent 2-IB, a selective inhibitor of neuronal and inducible nitric oxide synthase, holds great promise to reduce brain cell injury after cerebral hypoxia-ischemia and reperfusion, and improve long term outcomes in stroke, cardiac arrest and birth asphyxia.
The neuroprotective effects of 2-IB have been established in preclinical trials in four different animal models. Its excellent safety profile has been demonstrated in clinical trials in adults and newborns. 2-IB shows promising preliminary signals of clinical efficacy, which will be further investigated in larger clinical trials.
Indications
Stroke
Globally, more than 16 million people per year suffer from stroke. Stroke is the second leading cause of mortality (responsible for > 6 million deaths per year) and the second most common cause of disability. The absolute number of people with stroke and the global burden of stroke-related disability is high and increasing. The associated annual direct and indirect costs are estimated at more than 40 billion dollars in the US alone. About 30% of acute ischemic stroke is due to large vessel occlusion (LVO). LVO is disproportionately responsible for 60% of all stroke-related dependency and 90% of mortality. Standard of care is treatment with intravascular therapy (IVT) with recombinant tissue plasminogen activator ( rTPH ) to solve the clot and endovascular therapy (EVT) using thrombectomy to remove the clot. Aim of these treatments is to re-establish flow through the occluded artery and reperfusion of the brain. Although IVT and EVT improve clinical outcomes for 20% of AIS patients caused by LVO, more than half of AIS patients due to LVO still do not regain an independent lifestyle. Moreover, only 10% of LVO patients are symptom-free at follow-up despite combined IVT and EVT treatments. This leaves a great unmet need for AIS patients due to LVO.
Cardiac Arrest
In the Western World, each year more than half a million persons experience an out-of-hospital Cardiac Arrest (OHCA). This number is growing due to increasing obesity and lifestyle problems. Approximately 50% of OHCA-patients have sustained return of spontaneous circulation, but despite decades of research, median reported rates of survival to hospital discharge are poor (7.8%) and have remained virtually unchanged for the past 30 years. In survivors of Cardiac Arrest long neurologic deficits, cognitive defects, are present in 30 to 50% of patients, making Cardiac Arrest a large problem with a huge unmet medical need. Current treatment is temperature targeted management (TTM), in which the patient’s temperature is maintained stable at mostly at 36°C for 24 h. Effectivity of this treatment in comparison to the prevention of hyperthermia still needs to be proven. Therefore, new ways of neuroprotection are needed.
Birth Asphyxia
Neonatal encephalopathy (NE) following Birth Asphyxia (i.e. severe oxygen deprivation at birth) is one of the leading causes of neonatal death and adverse long-term neuromotor outcome in near term infants worldwide, resulting in cerebral palsy, mental retardation, visual impairments, and epilepsy. It is the cause of nearly 600.000 deaths worldwide every year, of which 99% occur in low- and middle income countries. The overall burden of NE is very high: about 2% of the total global burden of disease is being caused by NE (comparable to HIV and Malaria), resulting not only in about 1 million deaths worldwide, but also having a big impact on patients and families involved and therefore on society. Healthcare costs per life amounts to 1MUSD in the Western world. The only treatment proven to effectively reduce the sequelae of NE in the Western world, is the application of therapeutic hypothermia (TH, cooling). During TH the patient’s temperature is lowered to 33–34°C for 72 h. Despite this treatment, 45% of the neonates still has a bad outcome after 2 years. And although therapeutic cooling showed a significant decrease in handicap in high-income countries, studies in low- and middle income countries did not show positive results and even a higher mortality. Therefore, new ways of neuroprotection are needed.Our lead product 2-IB is currently in Phase II Clinical Trials for 3 indications